By Cameron Castelli, Contributing Writer
Cervical cancer – something no one wants to hear. However, for many people, it’s a reality they must face.
Cervical cancer is the fourth largest cancer in the world that affects women. A leading cause of this condition is the Human Papillomavirus Virus (HPV). HPV is a sexually transmitted infection, where in most cases will go away on its own. However, there are many other cases where it will lead to something more severe, such as cervical cancer.
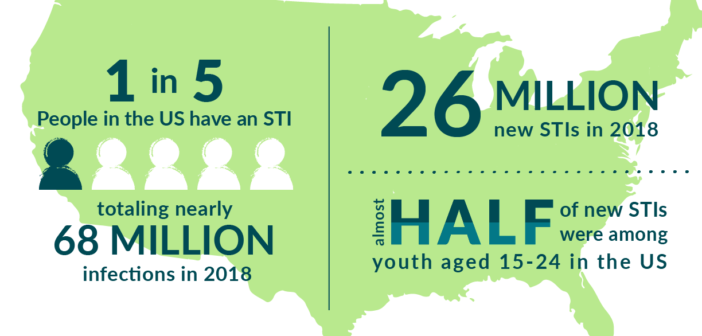
According to the CDC, “There were 43 million HPV infections in 2018, many among people in their late teens and early 20s.” It is estimated that 4,000 women die each year in the United States alone from cervical cancer.
Back in 2006, the CDC introduced an HPV vaccination that was proven 90 percent effective in preventing against this cancer, as well as HPV in both men and women. Normally, one would receive the shot at ages twelve to fifteen. The risks are very minimal, the worst being redness around the injection site for a couple of days and in some rare cases, a fever.
According to Dr. Cheryl Kozina, professor of cancer biology at Saint Leo University, “The HPV vaccine is a 2- or 3- shot series given over 6-12 months… No boosters are necessary because immunity/protection against the virus so far seems to be long-lasting, at least for the 18 years that it has been around.”
Kozina also stated that, “Things like fever or redness at the injection site are just evidence of the vaccine working! That’s your immune system responding to the antigen in the vaccine and raising a long-term immune response to it.”
With such a high success rate to such a fatal virus, why is it so hard to access?
In the United States it is administered free of cost by the VCF for those eighteen and younger; especially for families who are under Medicare, uninsured, or underinsured. However, in many low-income countries, the HPV vaccine becomes increasingly harder to afford.
The World Health Organization (WHO) already supplies the vaccine to more than one-hundred countries, but that does not mean it is affordable in each country. Turkey is one of these locations where the vaccine is supplied, but due to a 20-year high inflation rate, the vaccine costs 160 USD(which is more than half of the minimum wage income in Turkey). This was until a woman acted against this injustice.
Yagmur Varkal, a 24-year-old Turkish University student, made a class-action lawsuit against the Turkish government for affordable access to the HPV vaccination. In March of 2022, she won the landmark case. Her HPV vaccination was refunded at full cost.
The WHO’s global strategy to help aid in this case was endorsed at the seventy-third World Health Assembly.
According to the National Library of Medicine, “One target is 90% coverage of a full HPV vaccine sequence for girls, in addition to targets for high coverage of cervical cancer screening and treatment. To achieve this elevated level of vaccine coverage, the strategy underscores the importance of a sufficient supply of affordable HPV vaccines, introduction of HPV vaccination in countries that have not yet adopted the vaccine, and increased quality and coverage of vaccine delivery.”
Dr. Kozina concluded, “I’d encourage everyone to get vaccinated, regardless of gender. Preventing cancer is so much easier than treating it, and the fewer people who are susceptible to infection, the lower the risk to the overall population… Why wouldn’t you do what you can to prevent cancer? I see this as no different than quitting smoking or wearing sunscreen to protect from cancer.”